Abdurrahman F. Kharbat1§, Drashti Patel2§, Kiran Sankarappan3, Raja Al-Bahou2, Faisal Alamri4, Anjali Patel2, Rajvi Thakkar2, RyanD. Morgan5, Kishore Balasubramanian3, Brandon Lucke-Wold
1 Department of Neurosurgery, University of Oklahoma Health Sciences Center, Oklahoma City, OK, USA.
2 College of Medicine, University of Florida, Gainesville, FL, USA.
3 College of Medicine, Texas A and M University, Houston, TX, USA.
4 King Salman Hospital, Riyadh, Kingdom of Saudi Arabia.
5 Division of Neurosurgery, Texas Tech University Health Sciences Center, Lubbock, TX, USA.
6 University of Florida, Department of Neurosurgery, Gainesville, Florida, USA.
- A.K. and D.P. contributted equally to this paper
Correspondence to: Brandon Lucke-Wold, University of Florida, Department ofNeurosurgery, Gainesville, Florida, USA.
Received date: March 28, 2024; Accepted date: April 05, 2024; Published date: April 15, 2024
Citation: Kharbat AF, Patel D, Sankarappan K, et al. Timing of Agent Resumption and Therapeutic Targets in the Pathophysiology of Traumatic Brain Injuries, IJMRS @ PubScholars Group 2024;1(3):10-19
Copyright: ©2024 Kharbat AF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
ABSTRACT
An estimated 69 million people worldwide suffer from traumatic brain injuries each year. Direct head trauma can cause traumatic brain hemorrhage, which can be life-threatening if not treated quickly. Current studiessuggest the use of antithrombotic therapy for treatment, but the optimal duration of such therapy in neurosurgery remains controversial. This article critically reviews recommendations regarding the ideal timing of antiplatelet and anticoagulant therapy for diseases such as subarachnoid hemorrhage, subdural hematoma, skull fractures, brain contusions, and diffuse axonal injury. . Additionally, the role of these agents in the context of prosthetic valves and stents will be examined, and their effects on bleeding time and platelet aggregation will be evaluated. This review highlights possible directions for future research in this area and highlights the limitations inherent in the current literature. In the case of hemorrhage in TBI, the standard of care is to resume appropriate AAT at intervals to
reduce the risk of ICH, but timing and treatment vary among clinicians. Various studies have shown that restarting AAT reduces the long-term risk of thrombotic events and ischemic stroke. However, this benefit should be weighed against the risk of her developing ICH if AAT is restarted too soon. Timing of resumption of AAT should be determined based on multidisciplinary risk stratification considering patient risk factors and comorbidities that may predispose to thromboembolic complications due to prolonged discontinuation of AAT cessation.
Keywords:
Traumatic brain injury, Subarachnoid hemorrhage, Subdural hematoma, Aspirin, Clopidogrel, Antiplatelet and anticoagulant therapy.
Abbreviations:
TBI: Traumatic Brain Injury; SAH: Subarachnoid Hemorrhage; SDH: Subdural Hematoma; DAI: Diffuse Axonal Injury; ICH: Intracranial Hemorrhage; AAT: Antiplatelet and Anticoagulant Therapy; CT: Computerized Tomography; CATE: Secondary Cardiogenic Arterial Thromboembolism; DAPT: Dual Antiplatelet Therapy; CFR: Cyclic Flow Reduction; NOAC: Novel Oral Anticoagulants; DOAC: Direct Oral Anticoagulants
Introduction
Traumatic brain injury (TBI) refers to a devastating and complex medical condition that can cause death or severe disability [1]. TBI typically arises from direct physical trauma to the head, and it is alarmingly prevalent, with an estimated 69 million individuals worldwide suffering from TBI annually. Individuals in Asia and the Western Pacific experience the greatest burden of disease, including more severe symptomsand an increased mortality rate; however, Europe and North America have the highest number of recorded TBI cases [2].
Traumatic brain bleeds can occur in TBI due to various mechanisms, such as blunt force trauma, penetrating injuries, or acceleration-deceleration forces, leading to damage to the brain vasculature [3]. When traumatic brain hemorrhage occurs in association with traumatic brain injury, treatment of these injuries becomes even more complex. Two examples of traumatic brain hemorrhage commonly seen in TBI patients are subarachnoid hemorrhage (SAH) or subdural hematoma (SDH) [4]. SAH is most commonly caused by TBI, and traumatic SAH can lead to progressive neurological deterioration and increased patient morbidity and mortality [5]. Similarly, SDH is another possible consequence of TBI. 11% of mild to moderate TBIs and 20% of severe TBIs present with SDH [6]. SDH further compounds the challenges faced by patients with TBI, as evidenced by the 60% of patients who either die or become severely disabled following SDH [7]. This highlights the important role played by the cerebrovascular system in maintaining the health of nervous tissue. Damage to these blood vessels can lead to life-threatening complications. Along with SAH and SDH, other complications of TBI may also result in traumatic brain bleeds, including skull fractures, cerebral contusions, and Diffuse Axonal Injury (DAI). Notably, skull fractures resulting from TBI serve as a significant predictor of Intracranial Hemorrhage (ICH) [8]. One study by Lukas
Leitner, et al. assessed over 1700 patients with TBI and found a statistically significant correlation between skull fractures and ICH, as well as ICH-related outcomes [8]. Survival rates for patients with ICH remain distressingly low, with less than 50% of patients surviving to the one-year mark [9]. Those who do survive face the sequelae of complications resulting from traumatic brain bleeds, substantially compromising their quality of life. Cerebral contusion, another complication associated with TBI, is also linked to ICH. These contusions inflict permanent damage to cerebral tissue, stemming from the absorption of kinetic energy during direct head trauma. This trauma results in hemorrhagic lesions that can expand and worsen over time. Potential complications of contusions include seizures, hydrocephalus, severe disability, coma, and death [10]. DAI is also a TBI-related complication with many adverse effects, the most prominent of which is dysautonomia [11]. Overall, damage resulting from TBI varies gretly and has the potential to culminate into life-threatening traumatic brain bleeds.
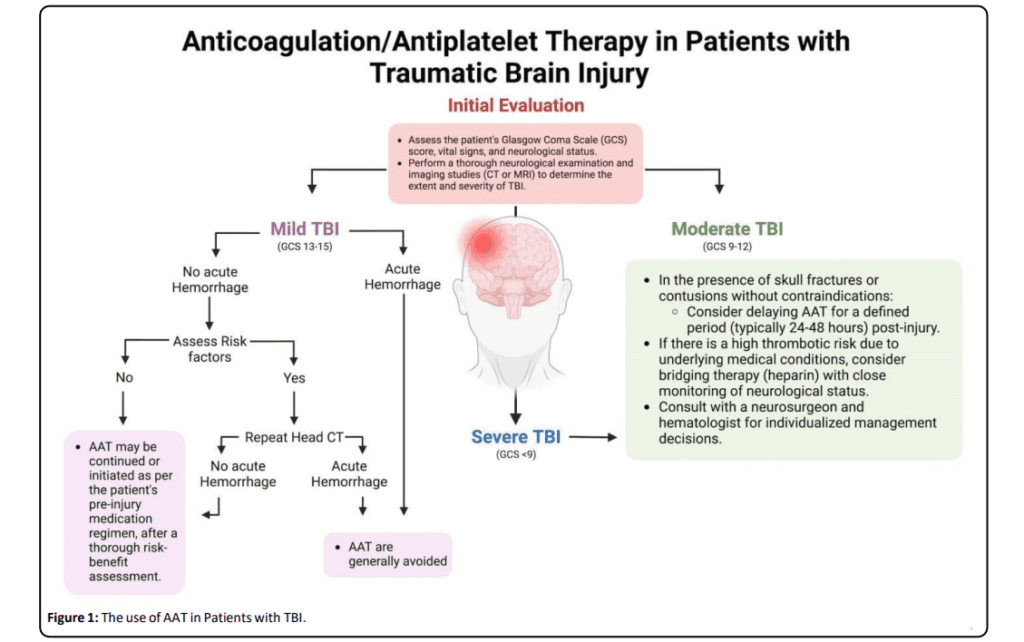
Traumatic cerebral hemorrhage can cause various sequelae that require emergency treatment to improve patient prognosis. Elevated blood pressure is associated with poor prognosis in traumatic cerebral hemorrhage, with an additional risk of contributing to hematoma expansion [12]. Although the use of antithrombotic therapy (AAT) is often indicated for the treatment of traumatic cerebral hemorrhage, there are a number of patient factors that need to be considered before initiating AAT, as shown in Figure 1. For example, given the high prevalence of traumatic brain injury in the elderly, many patients may have other comorbidities such as atrial fibrillation and deep vein thrombosis, and may be at risk for stroke or blood clots. AAT is required to reduce the risk of associated events [13-17]. The usefulness of AAT in other such diseases may complicate its use in the treatment of traumatic cerebral hemorrhage.
If a patient sustains a traumatic brain injury while taking AAT, these drugs can affect the blood’s ability to clot, increasing the risk of brain hemorrhage. Furthermore, excessive use of AAT may also falsely induce hypotension, which may reduce cerebral blood flow [12, 18]. Therefore, medical professionals should continue or use these medications during the acute phase of TBI treatment, striking a delicate balance between
preventing further intracerebral hemorrhage and minimizing the risk of blood clot-related complications. The benefits and risks of discontinuation must be carefully weighed [19]. This paper aims to review the literature to better ascertain the
appropriate duration of AAT in the context of traumatic brain bleeds. Our aim is to provide a comprehensive review of the current literature regarding the ideal duration of AAT administration after traumatic SAH and in acute or chronic SDH. Additionally, we examine the optimal duration of antiplatelet therapy and its impact on patient care in skull fractures, brain contusions, and DAI. We will also look at the impact of AAT on prosthetic valves and stents, and the impact of AAT on bleeding time and platelet aggregation. Our discussion will extend to the potential future implications for research concerning the utility of AAT in the context of traumatic brain bleeds, emphasizing the existing limitations within the current body of research on this topic.
AAT Duration in Traumatic SAH and Acute or Chronic SDH
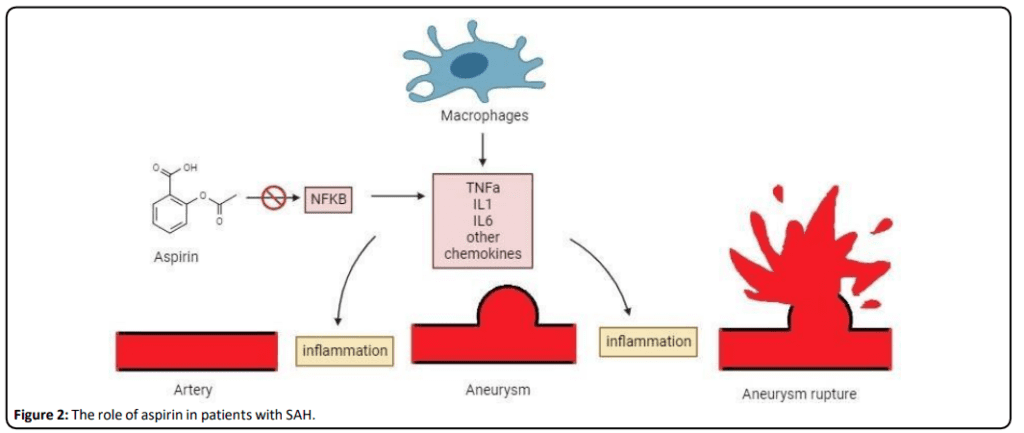
Researchers have long endeavored to elucidate and support the specific decision-making processes involved in deciding whether a patient should continue AAT after traumatic SAH [20]. This is an increasingly common topic, with many research papers finding an association between administration of the oral anticoagulant warfarin and increased risk of ICH, prompting further research on this topic [ 21 ]. Additionally, antiplatelet drugs such as aspirin are being studied for their role in preventing inflammation and aneurysm rupture, as shown in Figure 2.
The Role of Aspirin in Patients with SAH
The optimal timeframe for initiating oral anticoagulation therapy depends on numerous personalized patient factors. Taking this into account, Yan-Huang Li, et al. proposed a straightforward three-step model for determining the ideal timing of AAT administration [20]. • A patient’s risk of developing further thromboembolism or ICH is evaluated by considering a variety of factors, including history of atrial fibrillation, mechanical valve defects, and previous experience of deep vein thrombosis or pulmonary embolism. The decision to weigh the pros and cons of continuous anticoagulation therapy depends on the patient’s specific brain disease [20].
• The correct AAT is chosen, and the optimal timing for therapy is determined based on the conclusions drawn from step one. It is essential to recognize that the decision to initiate AAT should be a multidisciplinary effort, with the involvement of neurologists, neurosurgeons, and
interventional cardiologists, promoting a team-based approach to patient care [20].
• Clinicians take additional measures to manage any chronic comorbidities that the patient may be experiencing, such as hypertension, heart failure, or diabetes [20].
The first step of this model focuses on evaluating risk scores for thromboembolism and ICH, which can prove to be a complicated process. For instance, one study by Vivien H Lee, et al. established a simple scoring system known asthe HAIR score (Hunt and Hess score, age, intraventricular hemorrhage, rebleed)[22]. Thisscoring system,ranging from0 to 8, offersinsight into the various risks associated with SAH and was formulated based on data from 400 patients suffering from traumatic SAH and acute and chronic SDH. The study found that a higher HAIR
score was associated with increased hospital mortality among their patients [22]. Another study examined the aneurysmal rupture risk scores in patients with SAH in a large prospective study involving a cohort of 319 patients. Surprisingly, this team of researchers concluded that the aneurysmal risk scores did not correlate with a patient’s increased risk for mortality or intracranial bleeding [23]. This discrepancy between studies
calls for more research in the development of models that accurately predict a patient’s risk assessment in order to drawbetter conclusions regarding the duration of AAT.
The Optimal Timing for AAT in SAH and SDH
A retrospective study by Yana Puckett aimed to determine the best timing for resuming AAT in 256 patients with TBI between 2009 and 2012. The study reported that resuming AAT between 7 and 9.5 days after TBI may lead to fewer adverse events when compared to previous recommendations of 3-10 days. The study analyzed patient metrics,such as coagulation studies,type of TBI, treatment, and AAT resumption timing, and it evaluated patient outcomes during a six-month follow-up. Rates of complications were also assessed, including mortality, myocardial infarction, stroke, re-bleeding, venous thromboembolism, and pneumonia. Adverse events were least observed (10%) in the group restarting
AAT between 7-14 days, while the group not resuming AAT had the highest rate of adverse events (68.8%). One limitation of this study was low statistical power due to follow-up limitations and a patient cohort with shorter hospital observation periods and more benign brain injuries [17]. Further research should focus on patients with more severe TBIs with longer durations of hospitalization.Another review article by Jochen A. Sembill concluded that physicians typically initiated AAT as early as one week for patients without significant risk factors like atrial fibrillation
or a history of thromboembolism [24]. For patients with other relevant medical histories, the timing of re-initiation was adjusted based on individual risk factors. On the other hand, a survey of multiple neurosurgeons by Yan Xu et al. revealed a lack of consensus regarding the timing of re-initiating therapy, with 40% of physicians preferring to recommence treatmentbetween 14 days and 3 months after the initial injury [25]. In
conclusion, the literature offers varying recommendations, with some favoring re-initiation of therapy within one week, others suggesting a 1-2 week delay, and still others advocating for even longer intervals exceeding one month [17,24-29].
AAT indicationsfor other complications of TBI
Skull fractures, anterior cranial and temporal bone contusions, and administration of AAT after DAI are topics of ongoing research and clinical discussion. However, the lack of strong research such as randomized controlled trials has limited the availability of evidence-based clinical recommendations in this area [19]. Decisions regarding the management of AAT administration are complex and multifactorial, taking into
account the patient’s general health status, injury severity and location, and risk of thromboembolic and hemorrhagic events. Therefore, the approach to managing these patient cohorts is highly dependent on the empirical assessment and clinical experience of the physicians. This reliance on clinical judgment may contribute to the lack of an established protocol for determining the optimal time frame for resumption of AAT in patients after TBI [14, 17, 19].
AAT Indications for Minor TBI and Skull Fractures
The current literature presents a range of recommendations concerning the duration of AAT following TBI. For instance, in cases of minor skull fractures or minor TBI with negative Computerized Tomography (CT) images, there is typically no recommended reversal of AAT. Instead, it is advised to monitor the patient in the intensive care unit and perform repeat scans to rule out any potential bleeding [13,19]. If the subsequent
scans do not reveal any bleeding, the resumption of AAT may be considered within a matter of days to weeks, contingent upon other clinical and radiological assessments. However, the optimal duration of AAT for patients with skull fractures remains a topic of ongoing research. This highlights the need for further clinical trials and consensus guidelines to provide clearer recommendations to healthcare practitioners managing these complex cases [16].
AAT Indications for Severe TBI, Cerebral Contusions, and DAI
In cases involving severe TBIs characterized by extensive contusions or DAI, the potential benefits of AAT must be carefully weighed against the associated bleeding risks. This decision often requires multidisciplinary collaboration among neurologists, neurosurgeons, and hematologists to optimize patient outcomes while minimizing complications. However, rapid AAT reversal is recommended in patients with ICH, with platelet transfusion being the suggested approach for reversing aspirin or clopidogrel therapy [13, 19]. In cases of warfarininduced coagulopathies, effective treatment can typically be achieved with fresh frozen plasma and intravenous vitamin K. However, the use of recombinant activated factor VII in warfarin-associated traumatic ICH remains uncertain, mainly due to limited clinical benefits, cost considerations, and safety
concerns in trauma cases [13].
Albrecht, et al. conducted a retrospective investigation into the risk of adverse outcomes in TBI patients hospitalized for one year. They compared those who resumed warfarin therapy to those who did not, revealing a reduced risk of thrombotic events (RR, 0.77; 95% CI, 0.67–0.88) and hemorrhagic or ischemic strokes (RR, 0.83; 95% CI, 0.72–0.96) associated with warfarin resumption. However, warfarin resumption was also
linked to an increased risk of hemorrhagic events (RR, 1.51; 95% CI, 1.29–1.78). These findings suggest an overall net benefit in resuming anticoagulation for most patients [33].Another study, which included 3355 participants, reviewed the outcomes related to neurological deterioration or progression of hemorrhagic TBI on repeat head CT scans in patients who received anticoagulation within 60 days post-injury. The median administration time for anticoagulation after injury was found to be 9 days, and there were no indications of neurological decline attributable to the administration of anticoagulation; however, 6 patients exhibited an advancement of hemorrhagic TBI in follow-up head CT scans. Furthermore, multiple logistic regression analysis revealed that patients aged 65 and older were significantly linked to the advancement of hemorrhagic TBI following therapeutic anticoagulation (odds ratio, 15.2; 95% confidence interval, 1.1-212.7; P=0.04) [34]. Tykocki and Guzek, et al. also reported a relatively low risk of hemorrhagic complications in the early resumption of antithrombotic therapywithin3-17.5daysafterTBI. Furthermore, their findings indicate that the risk of such complications may be even lower when non-vitamin K antagonist oral anticoagulants
are used, compared to vitamin K antagonists [35].
Antiplatelet Therapies
The Effects of AATs on Prosthetic Valves and Stents
AAT therapy is also indicated for use in traumatic brain bleeds for patients with prosthetic valves and stents. For instance, one study by Makkar, et al. found that clopidogrel and aspirin therapy significantly reduced thrombus formation in ex vivo porcine models with deployed nitinol stents in external arteriovenous shunts. The study investigated the acute actions of these regimens and found that a combination of clopidogrel and aspirin demonstrated significant effects for reducing acute thrombus formation over the deployed stents, even at low doses. Aspirin showed synergistic effects when combined with clopidogrel, enhancing its anti-thrombotic effects, but models treated with aspirin alone had almost complete obliteration of the stent by the thrombus. Similarly, pigstreated with clopidogrel alone had an insignificant level of diminished thrombosis unless
given in relatively high doses when compared to the combined treatment regimen [36].
In another study involving a rabbit model, the combined regimen was assessed in ex vivo heart valves and compared with the acute effects of warfarin. The study found that clopidogrel and aspirin therapy resulted in a greater reduction of thrombus over the heart valves than warfarin or control groups [37]. Similarly, in a different experiment involving baboons, Harker, et al. examined the efficacy of clopidogrel and aspirin in preventing platelet depositions on externally placed arteriovenous shunts with stainless steel stents. The study examined the cumulative
effect of clopidogrel in inhibiting platelet depositions over six days on the hypercoagulable stent; it studied low doses of the clopidogrel and examined the additive effects of aspirin when combined with clopidogrel. The study also investigated heparin in an ex vivo placed stent, both alone and in combination with clopidogrel. The study demonstrated that heparin did not significantly reduce platelet depositions over the placed stent
unlessit was combinedwithclopidogrel. Thestudy also foundthat the combination of these regimens did not significantly increase the bleeding time when compared to clopidogrel alone [38]. McKellar, et al. also contrasted the effects of clopidogrel and aspirin with dalteparin in preventing thrombus formation over various periods of time. The study involved a post-mortemanalysis of thrombus size over implanted aortic valves. The
researchers studied swine for 30 days divided into three treatment groups: 1. combined treatment with clopidogrel and aspirin, 2. single treatment with clopidogrel, aspirin, or dalteparin, or 3. non-treated group. Swine receiving Dual Antiplatelet Therapy (DAPT) had a drastic reduction in thrombus size in comparison to the control group. Additionally, swine treated with single therapies had a larger thrombus size when compared to the DAPTs, but their effects were deemed to be insignificant. The swine receiving dalteparin had the largest thrombus size compared to the other treatment groups, followed by aspirin and clopidogrel. Dalteparin-treated swine had a thrombus size nearly three times larger than DAPTs.
DAPTs were also compared to the control group over 150 days. Mean thrombus size in the aspirin and clopidogrel combined group was significantly smaller than the control group, with a four times greater size reduction. Interestingly, there were no reported deaths due to thromboembolic events in the shortterm, long-term, or non-treated group [39]. Hence, it can be concluded that a combination of aspirin and clopidogrel is the most effective treatment for thrombi in prosthetic valves and stents.
The Effects of AATs on Intravascular Thrombosis
The debate regarding AAT also extends to the topic of intravascular thrombosis. For instance, one double-blinded randomized control trial studied two groups of cats receiving either aspirin or clopidogrel to investigate the incidence of Secondary Cardiogenic Arterial Thromboembolism (CATE). The researchers found that clopidogrel-treated cats had a significantly decreased likelihood of recurrent CATE and an increased median time for the event to occur. Additionally, the clopidogrel group was less likely to die due to cardiac causes [40].
The aforementioned study by Harker, et al. also found that although heparin and clopidogrel significantly reduced platelet aggregation on the placed stent, they did not decrease the platelet deposition on a vascular graft when compared to clopidogrel alone. Contrastingly, clopidogrel combined with aspirin diminished graft platelet depositions dramatically [38]. Another study measured the acute Cyclic Flow Reduction (CFR)
in the coronary arteries of pigs with induced unstable angina and its relation to clopidogrel and aspirin when used alone or combined. These researchers found that clopidogrel and aspirin together, even at low doses, exhibited rapid and effective action in decreasing the CFR whilst inhibition of platelet aggregation was delayed. In fact, aspirin or clopidogrel alone with the same doses did not show any effects at all [41].
The antithrombotic effects of clopidogrel, ticlopidine, and prasugrel were singly compared in rat models after induction of carotid arterial thrombosis in a different study. The study measured vessel occlusion time after induction of thrombosis and treatment in comparison to the non-treated group. Prasugrel displayed more potent and faster actions, compared to clopidogrel and ticlopidine, in keeping patent vessels and
reducing thrombus formation [42]. Moreover, these drugs were examined for their ability to prevent arteriovenous shunt thrombosis in rats; their results were strikingly similar to the previously mentioned study [42,43]. In another experiment involving rat models, aspirin, clopidogrel, enoxaparin, and heparin were compared with each other as single therapies or in combination with aspirin for the inhibition of CFR postinduction of carotid artery thrombosis. This study concluded that clopidogrel combined with aspirin was more effective than enoxaparin and aspirin or heparin and aspirin in the reduction of thrombus formation [44]. Combined therapy with aspirin and clopidogrel is more effective in treating intravascular thrombosis than other combination orstand-alone treatment regimens.
The Effects of AATs on Platelet Aggregation
Clopidogrel substantially inhibits ADP-induced platelet aggregation in a dose-dependent manner; however, it has no effect on collagen-induced aggregation. Contrastingly, aspirin prevents collagen-dependent aggregation in a dose-dependent pattern with a minimal effect on ADP-induced aggregation. A combination of both regimens resulted in a delayed effect on ADP-dependent aggregation without a significant effect on
collagen-induced aggregation [41]. On the other hand, prasugrel displayed stronger and faster inhibition of platelet aggregation in both mechanisms, and its inhibitory effects increased when combined with aspirin, even at low doses [45,46].
The Effects of AATs on Bleeding Time
The aforementioned study by H. J. Daykin, et al. compared bleeding time in association with the administration of AAT alone orin combination with aspirin. The tail bleeding times associated with heparin and enoxaparin were significantly increased at higher doses when compared to aspirin or clopidogrel alone. Combining anticoagulants with aspirin further increased bleeding time in contrast to the combination of clopidogrel and aspirin [44]. Similarly, rivaroxaban had a minor increase in bleeding time compared to clopidogrel with aspirin, but no statistically significant differences were found [47]. Clopidogrel and prasugrel also had no significant difference in the bleeding time [46]. Further research should focus on assessing bleeding time with combination therapies with larger sample sizes.
Ticagrelor, Prasugrel, and Clopidogrel
Another experimental study involved ex vivo and in vivo rat and dog models to compare ticagrelor therapy to clopidogrel and compounds 072 and 105, chemical compounds identical to prasugrel and its active metabolite, respectively. J.J.J. van Giezen, et al. found that ticagrelor has distinguishing chemical properties when compared to both prasugrel and clopidogrel. For instance, ticagrelor is an active compound that does not
need to be converted by the liver to exert its effects, unlike thienopyridines. Additionally, the high affinity of ticagrelor saturates active sites and leaves it able to more rapidly reach equilibrium when compared to clopidogrel and prasugrel [48]. Ticagrelor is also capable of reversibly binding to the active site,
unlike prasugrel and clopidogrel. Additionally, in vivo and ex vivo studies revealed no significant difference in bleeding time and thrombusformation between ticagrelor and prasugrel [49]
Future Implications for Research on the Use of AATs in Traumatic Brain Bleeds
Duality of Efficacy and Side Effects
The core concern when administering AAT in cases of traumatic brain bleeds revolves around the balance between potential therapeutic benefits and associated risks. These medications are invaluable for mitigating the danger of thrombotic events such as ischemic strokes. However, their mechanism of action also significantly elevates the risk of further hemorrhagic complications such as increased intracranial pressure, brain
herniation, neurological deficits, epilepsy, and cerebral edema [50]. While it is widely accepted that platelets regulate primary hemostasis, the impact of antiplatelet medications on subdural hematomas or subarachnoid hemorrhages remains an area of active investigation [51]. However, antiplatelet use has been associated with an increased risk of acute ICH post-head trauma, albeit with a low risk for delayed ICH [52-54]. Thus, immediate head CT imaging is recommended for all such patients [55]. In clinical scenarios where anticoagulation is crucial for the patient,
such as in atrial fibrillation or specific cardiac conditions, the decision to recommence treatment should be more meticulously calculated. Overall, the drugs that are currently in use in the context of traumatic brain bleeds are outlined in Table 1.


